By SAM McNEIL and SYLVIE CORBET
BRUSSELS (AP) — Germany, France and other European countries vowed their unwavering support for Ukraine on Monday as their diplomats scrambled to finalize new sanctions on Russia and a massive new loan for Kyiv ahead of the fourth anniversary of a war that has left an estimated 1.8 million Russian and Ukrainian soldiers dead, wounded or missing.
They also struggled once again to persuade Hungary to support the latest EU efforts to help Ukraine and to make Russia pay an economic price for the all-out war that it launched against its neighbor on Feb. 24, 2022, and which shows no signs of ending.
EU diplomats set to meet Board of Peace director over Gaza’s future
Today in History: February 23, American speedskater first to win 5 gold medals in a single Olympics
Mexico fears more violence after army kills leader of powerful Jalisco cartel
China, India among winners after US court blocked Trump tariffs
Kim reelected to top post of North Korea’s ruling party as it hails his nuclear buildup
Hungary, seen as the most pro-Russian member of the EU, threatened on the weekend to veto both the sanctions and a major loan meant to help Kyiv meet its military and economic needs for the next two years.
German Chancellor Friedrich Merz marked what he called “four monstrous years of war” at a pro-Ukrainian event in Berlin on Monday.
“I appeal again to our European partners — do not let up in your support, in our common support, for Ukraine,” Merz said. “We are standing at a crossroads that could decide on the well-being of our whole continent.”
“No one can say today whether the weapons will fall silent in Ukraine in six weeks, in six months or even later,” Merz said. “But we are working for them to fall silent as quickly as possible.”
In Paris, French President Emmanuel Macron declared that “our determination to continue supporting Ukraine is unwavering.” He met with Finland’s President Alexander Stubb, another staunch supporter of Ukraine who urged European allies to raise the costs on Russian President Vladimir Putin.
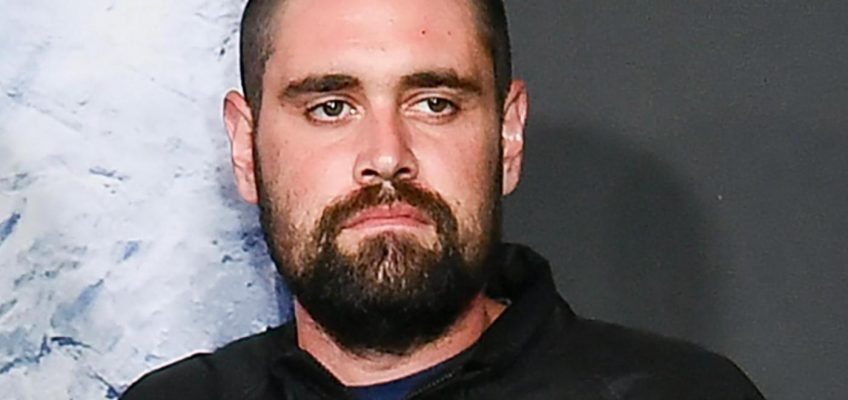
Hungary’s Foreign Minister Peter Szijjarto arrives for a meeting of EU foreign ministers at the European Council building in Brussels, Monday, Feb. 23, 2026. (AP Photo/Virginia Mayo)
EU diplomats grapple with Hungary’s objections
Many EU leaders had hoped to move forward on the sanctions and loan before the anniversary of the war’s start Tuesday.
But EU foreign policy chief Kaja Kallas said that the foreign ministers of the EU’s 27 member states meeting in Brussels would likely not agree Monday on the 20th package of sanctions targeting Russia’s shadow fleet and energy revenues.
Hungary on the weekend threatened to block the sanctions and to obstruct a $106 billion loan for Ukraine which it had previously agreed to, saying it would stand firm until Russian oil deliveries to Hungary resume.
Russian oil shipments to both Hungary and Slovakia have been interrupted since Jan. 27 after what Ukrainian officials say were Russian drone attacks that damaged the Druzhba pipeline, which carries Russian crude across Ukrainian territory and into Central Europe.
Hungarian Prime Minister Viktor Orbán doubled down Monday on an unsubstantiated allegation that Ukraine is deliberately holding back shipments of Russian oil, and accused Kyiv of seeking to topple his government. He referred to the oil supply disruptions as a “Ukrainian oil blockade” led by President Volodymyr Zelenskyy.
“No one has the right to put our energy security at risk,” Hungarian Foreign Minister Péter Szijjártó said as he sparred with journalists in Brussels ahead of the meeting.
Nearly every country in Europe has significantly reduced or entirely ceased Russian energy imports since Moscow launched its full-scale war in Ukraine. Yet Hungary and Slovakia, both EU and NATO members, have maintained and even increased supplies of Russian oil and gas, and received a temporary exemption from an EU policy prohibiting imports of Russian oil.
Germany’s Foreign Minister Johann Wadephul speaks with the media as he arrives for a meeting of EU foreign ministers at the European Council building in Brussels, Monday, Feb. 23, 2026. (AP Photo/Virginia Mayo)
Raising the pressure on Russia
Some European leaders stressed that the most effective way to get Russia to agree to peace in Ukraine is to raise the cost to Russia of continuing the war.
“This war will only end when Russia no longer sees any sense in continuing it; when Russia can no longer expect more territorial gains; when Russia’s costs for this madness have simply become too high,” Merz said. “We must dry up Moscow’s war financing.”
In Paris, Finland’s leader argued that Russia’s war in Ukraine was a “strategic failure” as he made the case for ratcheting up pressure on Putin.
“It is also a military failure — he is now losing many soldiers — and, on top of that, it is an economic failure,” Stubb said, speaking in French. “Putin is not winning this war, but he cannot make peace.”
The EU has already sent Ukraine $229.8 billion in financial assistance while at the same time squeezing Russia’s key energy exports.
Hungary’s Foreign Minister Peter Szijjarto speaks with the media as he arrives for a meeting of EU foreign ministers at the European Council building in Brussels, Monday, Feb. 23, 2026. (AP Photo/Virginia Mayo)
Hungary’s looming election hangs over EU talks
Facing a crucial election in less than two months, Orbán has launched an aggressive anti-Ukraine campaign and accused the opposition Tisza party, which leads in most polls, of conspiring with the EU and Ukraine to install what he called Monday a “pro-Ukraine government aligned with Brussels and Kyiv.”
Poland’s Foreign Minister Radosław Sikorski said he believed Hungary’s veto threat could really be about Orbán’s fierce fight to hold onto power.
Orbán, the EU’s longest-serving leader, will face off in April against the greatest challenge to his power since he took office in 2010.
“I would have expected a much greater feeling of solidarity from Hungary for Ukraine,” Sikorski said in Brussels. “The ruling party managed to create a climate of hostility towards the victim of aggression. And then it is now trying to exploit that in the general election. It’s quite shocking.”
European Union foreign policy chief Kaja Kallas arrives for a meeting of EU foreign ministers at the European Council building in Brussels, Monday, Feb. 23, 2026. (AP Photo/Virginia Mayo)
Hungary had already agreed in December to the EU loan, and it is unclear how it can backtrack now.
“We must release that. We must find an agreement between the member states because Ukraine needs this money heavily,” said Margus Tsahkna, the foreign minister of Estonia, which on Tuesday will celebrate the 108th anniversary of its independence from then-Soviet Russia in 1918.
Corbet reported from Paris. Associated Press writers Justin Spike in Budapest and Geir Moulson in Berlin contributed to this report.