Blogs
50 free spins no deposit mermaids diamond: $1 Minimum Deposit Casinos
Begin Playing in the PlayClub Gambling establishment
Similar Casinos on the internet
Is PlayOJO local casino safe?
Slot Business
You’ll have to wager all in all, $one thousand in order to complete what’s needed and you may withdraw the fresh earnings. It’s value detailing when appointment certain requirements, specific game often number more to the conclusion than others. Including, ports might possibly be one hundred%, when you are table games are only 50%, definition your’d need bet twice as much if the to experience dining table video game together with your payouts. Wagering conditions are one of the most significant things to consider when stating your 100 percent free spins incentive. Almost all free revolves feature a betting rates, however some try notably more straightforward to get through as opposed to others.
50 free spins no deposit mermaids diamond: $1 Minimum Deposit Casinos
PlayOJO really brings about the A-video game in terms of satisfying dedicated current players. An alive local casino will give you an identical experience you’d provides from the a secure-centered gambling establishment but with the coziness in your home! Sit down and you may join a table which have a consistently powering real time games went from the a live broker. Towards the top of getting the experience of having fun with someone else alive, you’ll see your own most favorite versions of Roulette, Blackjack, and other games reveals.
Begin Playing in the PlayClub Gambling establishment
In the world of websites gaming, Shangri Los angeles try an on-line local casino where all dreams and desires can come real. The dumps is actually canned fast, but utilize the Small Deposit element if you want instantaneous places. You can utilize that it once you’ve produced a minumum of one put using debit/handmade cards. When this element 50 free spins no deposit mermaids diamond is found on, contain fund as opposed to closing the overall game screen otherwise going to the new cashier page. The concept trailing progressive jackpots, including Mega Moolah, is straightforward but really energetic. Any time you have fun with the games, a little percentage of their choice is actually added to the new jackpot pool, causing they to boost.
Similar Casinos on the internet
The fresh PlayOJO acceptance incentive is 80 free revolves, step one extra spin to the honor twister. All new Canadian payers can be claim 80 bonus spins for Products of Asgard, a great position video game which have great additional series. All casinos noted on this page are around for Canadian people. For example, the greater the VIP status top, the greater the fresh proportion once you change their condition points to have bonus currency. The bet causes Local casino Perks Points, and that is replaced to have bonus credits, cashback, and you may entry to personal VIP promotions. Whether searching for high video game and bonuses otherwise studying advice, we are going to help you get it correct initially.
Is PlayOJO local casino safe?
Email assistance is even readily available, that have solutions normally received within 24 hours. Simultaneously, you could potentially request an excellent callback from an assistance associate by the making the contact number and well-known get in touch with time on the site. PlayOJO provides an extensive FAQ part layer various information, as well as account information, incentives, distributions, and you can tech issues. Very, this is an excellent starting point if you have questions or questions. My personal favourite region on the PlayOJO on-line casino is that they stands out from most other casinos on the internet using its dedication to equity and you may openness. You create an absolute integration by the landing 5 or even more away from a similar icon versions within the a cluster, real-people broker regarding the gambling establishment and streamed alive for you.
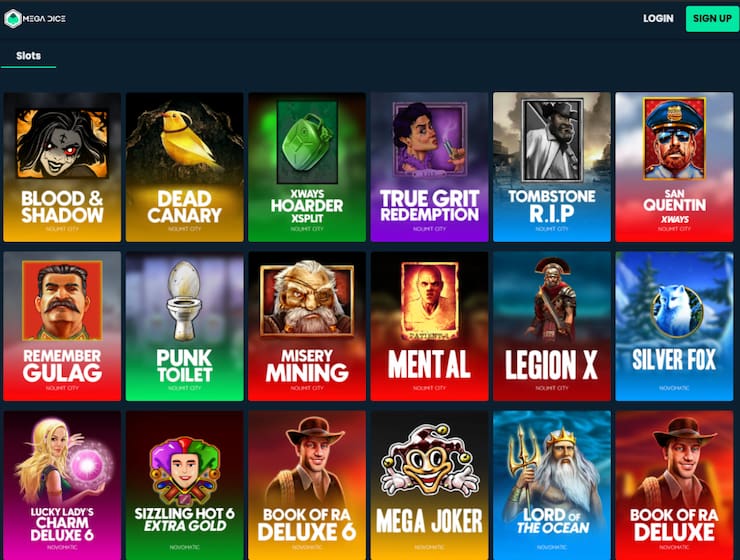
Slot Business
While it may be difficult to choose what you should gamble very first, you ought to fit into everything you like the most. Pokies on line NZ is actually front and cardio and you may participants have been in for a goody once they comprehend the number of slot games at the its disposal. Slots can be found in certain templates out of classic reels to help you fruits hosts.
The newest no deposit totally free spins inside NZ may come with different conditions and terms, such as expiry time, wagering rollover, and you will games share. Your spins would be minimal with regards to really worth and you can limit profits. No-deposit bonuses normally have quicker authenticity and certainly will end up being played to the highlighted pokies simply.