Since it was signed into law on July 4, West Texas Republican Congressman Jodey Arrington has been broadly praised by allies for his stewardship of the so-called One Big Beautiful Bill Act (OBBBA). U.S. House Speaker Mike Johnson called Arrington, who chairs the powerful House Budget Committee, “one of the most effective and consequential members of Congress.” And Arrington has wasted no time touting his victory in West Texas, proclaiming it to be a “game changer for Rural America” and “a big beautiful win for West Texas.” He’s argued the so-called entitlement cuts to Medicaid, the Affordable Care Act (ACA), and the Supplemental Nutrition Assistance Program will “root out waste and fraud.”
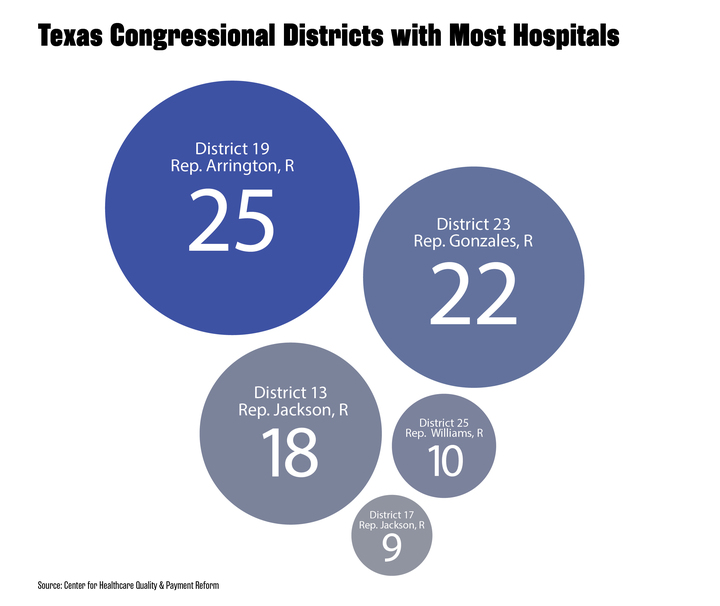
But many of his constituents in Congressional District 19—a vast, deeply red rural district that includes over 30 counties—stand to lose access to both their healthcare and their local hospitals under the massive tax-and-spending bill, which will slash Medicaid and ACA spending by more than $1 trillion and knock 10 million more people off of insurance nationwide over the next 10 years, according to Congressional Budget Office estimates. Arrington’s district is home to more rural hospitals than any other in Texas, and roughly a quarter of those are at risk of closing under the new law, according to a recent study. Six of the 25 hospitals in the 19th are at risk of closing, according to a June study by the Cecil G. Sheps Center for Health Services Research at the University of North Carolina. Using data from 2020 to 2022, the study defined at-risk rural hospitals as those with three consecutive years operating with a negative profit margin or those which receive a disproportionately large share of revenue from Medicaid.
Losses to rural hospitals from changes to Medicaid funding under the new law may be blunted by a $50 billion rural health fund that was added as a last-minute concession to rural members. The National Rural Health Association projected that the major hit Texas rural hospitals would take under the new law would shrink from an estimated loss of $1.2 billion to $407 million after the rural fund is applied over the next five years. But both the federal Centers for Medicare & Medicaid Services and state governments will have wide latitude on how to use the funding.
That’s left rural hospital administrators in Arrington’s district uncertain about the future of their facilities—and how the new law will affect them. Dennis Fleenor, the leader of the hospital in Muleshoe in Arrington’s district, has concerns. “By the time CMS and the state and everybody else get their fingers in that small slice of pie,” Fleenor said, rural hospitals like the one he runs may not get much money from the rural health fund.
Arrington did not respond to the Observer’s questions about the healthcare impact residents and hospitals in his district may face under the OBBBA. Arrington has served as the district’s representative since 2017 after a career that included working for a private healthcare company, for Texas Tech University, and as an aide for George W. Bush in the Texas Governor’s Office and the White House. Arrington has served as chairman of the House Budget Committee, one of the most influential positions in Congress, since 2023. He’s also served on the House’s Rural and Underserved Communities Health Task Force since 2019.
(Texas Observer)
The 19th Congressional District hugs the New Mexico border on the west and crosses central West Texas past Abilene to the east. Anchored by Lubbock and Abilene, the district is largely rural, featuring 17 million acres of farmland that produce a fifth of the state’s total agricultural sales and more cotton than any other district in the country. It’s also mostly white and deeply conservative. Around 15 percent of the district’s residents are uninsured, according to 2023 census figures, which is nearly on par with the statewide rate—the highest in the nation. Many residents in Arrington’s district rely on public healthcare: 131,000 or 18 percent of the district population are enrolled in Medicaid. Statewide, 16 percent of residents are enrolled.
Ten percent of the district’s population is enrolled through the ACA marketplace, lower than the state’s 15-percent rate, according to a study by the health research and policy organization KFF. The tax-and-spending bill doesn’t extend ACA tax credits that expire at the end of the year and thus will cause insurance premiums to surge for the vast majority of current enrollees. KFF estimates the removal of the tax credits and added hurdles to enroll in the ACA could cause 1.7 million Texans to lose ACA coverage.
Because Texas never expanded Medicaid under the ACA, the state will not have to impose work requirements on Texas’ Medicaid patients or reduce its provider tax rate, which will be a requirement under the new law starting in 2027. However, the OBBBA did freeze the provider tax rates states use to finance Medicaid on July 4, making it more difficult for states to increase their own funding for the program.
Dr. Adrian Billings, a longtime West Texas community physician and associate dean of the Rural and Community Engagement Division at Lubbock’s Texas Tech Health Sciences Center, said that hospitals are required by law to provide emergency care to patients regardless of whether they can pay. But unlike urban hospitals that serve a higher volume of patients and can better afford to offset the costs of treating uninsured patients, increases in uninsured rates can quickly dig rural hospitals into bigger financial holes.
“It is harder for a rural hospital to absorb when somebody without insurance shows up in the emergency room or needs to be hospitalized,” Billings said. “There’s just not much fluff at all left in a rural hospital’s margins to suffer any significant hit to their collection.”
The Mitchell County Hospital District serves the county of nearly 9,000 in the southern area of Arrington’s district, situated between Big Spring and Sweetwater. CEO Michelle Gafford told the Observer that the county hospital projected to lose about $700,000 in Medicaid funding, or roughly 3 percent of its 2026 fiscal year budget. “The cuts are going to hurt everybody; but they are not as crucial as they once would have been,” Gafford said, since the hospital’s share of Medicaid patients has steadily transferred to privately run managed care organizations. In the 13 years Gafford has worked at the hospital, it’s made a profit in only one year. The hospital is designated as a critical-access hospital, which allows it to receive Medicare reimbursements at roughly the same amount of the cost of services. However, other insurers, particularly Medicare Advantage and other private insurers routinely underpay or deny coverage for services, leaving rural hospitals, like the Mitchell County Hospital District, persistently in a financial hole.
More recent data gathered and analyzed by the Center for Healthcare Quality and Payment Reform shows that 11 rural hospitals in Arrington’s district now have had a negative total margin in the most recent three consecutive years with available data—representing over half of the 19 total such hospitals in the state. According to that data, three hospitals in the district have 20 percent or more of the hospital’s patient costs associated with Medicaid services. That includes the Muleshoe Area Medical Center.
Since the 1980s, the Muleshoe area hospital, located in the sparse western Panhandle near the New Mexico border, has gone through its ups and downs as its owners changed from one group to another. According to the hospital’s website, after one national company bankrupted the hospital in 1987, a Muleshoe physician named Bruce Purdy kept it running by seeing patients, cleaning its bathrooms, repairing the facilities, and even sleeping in his clinic to attend to late night emergencies. Dennis Fleenor, a Lubbock transplant, now runs the critical-access hospital on a shoestring budget. “It’s a struggle everyday. But we’re here to take care of our community, and we will take care of our community whatever challenges we face,” he told the Observer. But he said that Congress can go a long way to help rural hospitals by making insurers fully reimburse hospitals for patient service costs. Even though the hospital reported an average of 20 percent of the hospital’s patient service costs over the last two years were related to services for Medicaid patients, Medicaid paid the hospital for only 18 percent of those costs.
Between 2005 and 2025, 25 rural hospitals in Texas have closed, the most of any state, according to the center’s analysis. In CD-19, two rural hospitals closed during that time and at least six of the district’s 30 counties in the district already lack hospitals. In Jones County, north of Abilene, there once were three hospitals. In 2018, Stamford Memorial Hospital closed because it didn’t have enough in-patients. The following year, nearby Hamlin Memorial Hospital closed, leaving only its medical clinic and EMS services open. By 2023, Anson General Hospital was hanging by a thread with $1.9 million in outstanding debt. At that point, its board decided to convert the facility to a “Rural Emergency Hospital.” That federal designation was established under a 2021 law that Arrington helped spearhead as a last resort for rural hospitals; in order to qualify for federal grants, those facilities must eliminate in-patient services. Texas now has five Rural Emergency Hospitals statewide; two, Anson General Hospital and Crosbyton Clinic Hospital, are in Arrington’s district.
Vance Boyd, an Anson-based cattleman, pro bull rider, and general contractor, told the Observer he remembers when Anson General Hospital was “thriving, productive, and employed a lot of people.” But he says it’s now “a triage center to get you to a bigger market.” As a cancer survivor, he travels roughly 24 miles to Abilene to see his doctor. “If you’re having a health emergency in a more remote area, you’re pretty much on a dice roll whether you’re going to make it,” Boyd said.
Gaines County, which borders New Mexico, was the epicenter of Texas’ recent measles outbreak. Since January, the outbreak has led to 762 cases, 99 hospitalizations, and two deaths statewide, according to the Texas Health and Human Services. Eighty-one percent of the cases occurred in counties within Arrington’s district. Cash-strapped county hospitals with crumbling infrastructure in the surrounding area lacked the space to test for measles or beds to treat patients, the Texas Tribune reported.
Frustrated with the healthcare system, the “death spiral” of rural hospitals, and “AWOL” politicians, Boyd, a conservative Republican, ran against Arrington unsuccessfully in the 2020 and 2024 GOP primaries. His campaign centered, in part, around the need to expand Medicaid in Texas.
“When you live in an area where the average income is low and many are on some sort of government assistance, to expect everybody to have a premium healthcare plan is not realistic,” Boyd said. “I feel like our representative didn’t fight for us.”
Arrington, meanwhile, has his sights set on even further cuts to Medicaid. In mid-July, less than two weeks after he helped pass the OBBBA, Arrington told Bloomberg News that he would be seeking to pass deeper cuts to Medicaid, along with Medicare cuts that he had tried and failed to get locked into the Big Beautiful Bill. Among Arrington’s goals for a budget bill sequel this fall are to cut the federal reimbursement rate to penalize states that expanded Medicaid coverage under the ACA and reduce Medicare reimbursements to hospitals by paying the same rate regardless of the provider.
“I think we will do one before the end of the year,” Arrington told Bloomberg News. “It’s going to be a more targeted set of reforms.”
The post West Texas Congressman’s ‘Big Beautiful’ Cuts Could Harm Rural Hospitals in His District appeared first on The Texas Observer.

Leave a Reply